SOCIAL DETERMINANTS OF HEALTH
Improving Maternal and Infant Health requires more than clinical care . . .
The word “health” describes our physical condition, but it is also a reflection of how we live. Where we were born, how we learn, work, shop, play, and age all affect our quality of life. These health-influencers are called Social Determinants of Health (SDoH).
SDoH issues affect what we eat, our sense of security, social engagement, and family support. They can enhance or degrade our well-being by affecting access to healthcare, fresh food, and a living space free from toxins and other physical threats. Solving for the broad array of SDoH needs is critical to maintaining a continuity of care for women, infants, and their families – across both Medicaid and commercial health plan populations.
The integration of Utilization Management (UM) and Case Management (CM) enables collaboration, coordination, and communication across multiple clinical disciplines and departments – and with local social resources and services. Incorporating SDoH into the clinical ecosystem facilitates healthy outcomes for women and infants by helping families address the problems that impact their daily lives.
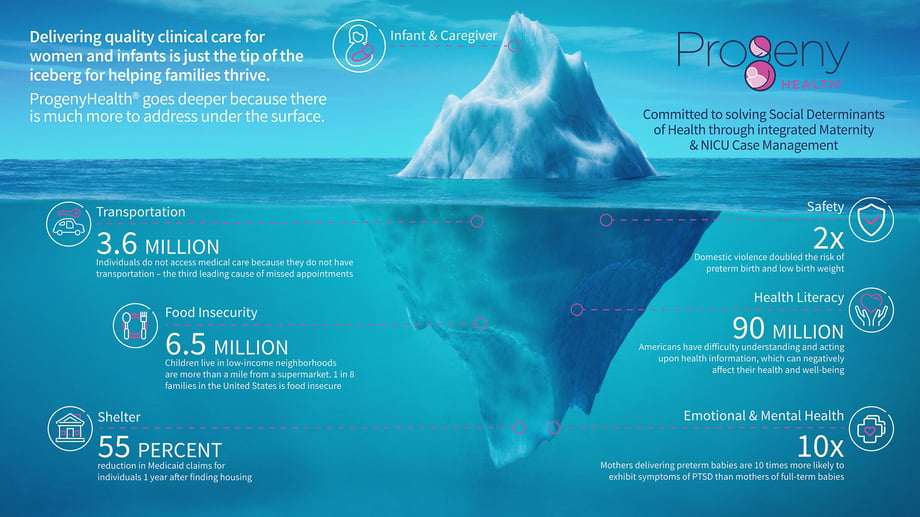
The Social Determinants that affect families include:
Health Literacy
A new parent or caregiver’s health literacy – the capacity to obtain, interpret, and understand basic health information – can affect their ability to follow recommendations to safeguard infants from illness or injury and promote their well-being. Studies indicate that 90 million Americans have difficulty understanding and acting upon health information, and, that this issue is compounded when language barriers are involved.
Twenty percent of caregivers in one study demonstrated low health literacy and had difficulty managing services. Supporting and educating caregivers to achieve a higher level of health literacy helps them communicate with providers more efficiently and navigate the support system and resources they need.
Food Insecurity
1 in 8 Americans faces food insecurity. 6.5 million children live in low-income neighborhoods that are more than a mile from a supermarket. Children who live in households that are food insecure are likely to be sick more often, recover from illness more slowly, and be hospitalized more frequently. Food insecurity can affect children in any community, not only traditionally underserved ones.
 Emotional Health/Mental Health
Emotional Health/Mental Health
1 in 8 of all visits to US emergency departments are related to mental and substance use disorders. Parents are at particular risk for postpartum depressive symptoms, anxiety, and stress after their newborns are discharged from the hospital
Shelter
Infants born during a period of unstable housing have higher rates of low birth weight, respiratory problems, fever, and other common conditions. They also experience longer neonatal intensive care unit stays, more emergency department visits, and higher annual spending.
As cited in this article, one study found a 55 percent reduction in Medicaid claims for individuals one year after finding housing, and others have also shown that access to stable housing shortens hospital stays by 29 percent and reduces emergency department visits by 24 percent.
 Community
Community
Where you live matters to your health. 80% of health outcomes are impacted by socio-economic conditions, health behaviors, and one’s physical environment. Additionally, studies show that integrating social/community services with medical services can be ten times more effective than waiting for families to visit health services.
Transportation
The availability and accessibility of public transportation impact access to employment, healthy food, health care, and other drivers of health and wellness. The American Hospital Association reported that 3.6 million individuals – regardless of payer status – are unable to access medical care because they lack transportation.
Interpersonal Safety
Domestic violence by a partner or ex-partner during pregnancy increases the risk of preterm birth, low birth weight, and small-for-gestational-age babies. This risk is increased further for women who experienced two or more types of domestic violence during their pregnancy.
Data indicates a direct correlation between SDoH and infant mortality (IM). Studies reported in the Journal of Health Care for the Poor and Underserved show:
- Poverty – Individuals with the lowest incomes have the highest risk of infant death. For example, African Americans and non-Hispanic Whites in the highest poverty tier are at greater risk of sudden infant death syndrome (SIDS). Poverty has also been shown to be a contributor to acute and chronic stress, which have an impact on infant mortality.
- Breastfeeding – Studies found that breastfeeding for any duration decreased the likelihood of SIDS.
- Education – Several studies have found education to be a protective factor against infant mortality. The odds of infant mortality were higher for non-Hispanic Black women with low levels of education than for their non-Hispanic White counterparts.
- Maternal Health – Multiple studies have demonstrated the increased risk of infant mortality from maternal conditions such as diabetes and hypertension.
- Smoking – Maternal smoking in the prenatal and postpartum periods increases infant mortality. Second-hand smoke in the infant’s environment is also associated with an increased risk of infant death, including unexplained infant death (SUID), SIDS, and infectious diseases.

- Safe Sleep – Unsafe sleep positions (i.e., prone position) increase the odds of infant mortality and are particularly associated with increased risk of SIDS. Some segments of the population are less likely than others to follow physician recommendations. Access to cribs and bassinets is another SDoH factor in sleep-related infant deaths.
- Access to Healthcare – Rural areas and poor neighborhoods often have few medical specialists, such as obstetricians and neonatologists. Residing in a region with more specialists lowers the risk of neonatal mortality. The level of hospital care also plays a significant role, especially the quality of healthcare facilities. One study found that African American women who deliver in NYC hospitals have overall higher infant mortality rates.
- Social & Environmental Factors – Neighborhood poverty and racial segregation are associated with higher rates of infant mortality. Family imprisonment rates increase infant mortality, as does income inequality. Exposure to air pollution (i.e., carbon monoxide, nitrogen dioxide, and fine particulate matter) in the months preceding an infant’s death was significantly associated with infant mortality.
ProgenyHealth’s Case Managers and Social Workers provide steady guidance and problem-solving for parents and caregivers of infants from conception through the first year of life, and beyond. Here are specific ways we reduce healthcare costs and enhance a family’s health and well-being by connecting them to providers and local resources who can deliver:
Social Services
-
- Securing housing
- Short-term hotel stays
- SSDI benefits
- Child Protective Services
Medical Support
-
- Community health benefits
- Health plan benefits
Addiction Support
-
- Medication-Assisted Treatment (MAT) support
- Smoking cessation
- Behavioral health
Food Insecurity
-
- WIC benefits
- Supplemental Nutrition Assistance Program
New Mother Skills
-
- General newborn care (feeding, diapering, temperature taking)
- Lactation support
Infant Health
-
- Vaccinations
- Diapers and formula
- Early intervention evaluations
- Monitoring developmental milestones
Transportation & Appointments
-
- Transportation to appointments
- Pediatric primary care arrangements
Despite a continuous endeavor by health plans to manage costs and improve outcomes, a key lever is often beyond their grasp: Social Determinants of Health.
For health plans with diverse member populations, costs attributed to SDoH often show up in emergency department (ED) usage. Over the last three decades, the number of ED visits has continued to increase, reaching a 10-year high for all age groups and especially for members in the 45-64 year group. Health plan members with chronic conditions often resort to the ED for health issues that could have been better managed through regularly scheduled care. For this reason, ED overutilization, as well as SDoH-related readmissions, place a financial burden on health plans that is largely preventable.
Compared to other developed nations, the US ranks last for health outcomes, equity, and quality, despite having the highest per capita spending on health. Social factors play a significant role in this disparity – from lack of access to affordable health care, health literacy, concerns about finances, and the long list of other SDoH.
There are many reasons why a member would visit the ED. Unlike with a primary care physician, or an engaged case manager, EDs are not set up to deliver preventive post-NICU care and this results in fragmented care in general. And, while hospitals and health plans have social workers, they don’t typically have the dedicated infrastructure to address SDoH.
Breaking the cycle of preventable ED visits would require health plans to address social needs and deliver whole-person care directly. But, unless SDoH is part of an organization’s primary mission, managing social needs is a challenge.
The key is to integrate social care into the delivery of medical care
There are more than 400,000 social service organizations in this country that work with disenfranchised populations and stressed individuals. These organizations have the boots on the ground and local resources to address issues connected to food, shelter, childcare, domestic violence, behavioral health, and more. But unfortunately, most social service organizations don’t have the technology, processes, contracting, and reporting that health care organizations require.
A proactive approach is critical to solving SDoH concerns and delivering successful outcomes. ProgenyHealth’s needs assessment begins as early as the detection of a pregnancy. Identifying members with social needs helps to avoid the costs that can mount from delayed interventions.
ProgenyHealth provides the infrastructure needed to integrate SDoH case management into the broader clinical ecosystem. We maintain seamless coordination between clinicians and social service professionals to facilitate timely solutions to SDoH challenges. By guiding new families through these challenges, our case managers help families utilize appropriate health care resources, avoid unnecessary ED visits, and build a solid health footing from a managed continuity of care.
 ProgenyHealth’s Utilization Management, Case Management, and Payment Validation and Assurance programs are tightly integrated into a comprehensive solution to serve infants, families, providers, payers, and employers.
ProgenyHealth’s Utilization Management, Case Management, and Payment Validation and Assurance programs are tightly integrated into a comprehensive solution to serve infants, families, providers, payers, and employers.
Our proven Process, technology Platform, and our experienced team of People enable our partners to reduce NICU case costs and sustain those savings post-discharge by identifying and solving SDoH issues impacting these families.
Our Process:
From pregnancy to a potential NICU admission, through the first birthday and beyond, our focus is on infant health outcomes and the well-being of families/caregivers by engaging in collaborative care conversations with providers and affirming standardization of care that follows recognized best practices.
-
-
Utilization Management: Our UM team monitors the infant’s progress telephonically and maintains contact with the hospital staff, forging strong peer-to-peer clinical relationships with them to evaluate and help ensure the quality and efficiency of the care being delivered.
-
Case Management: Our case managers advocate for the infant by engaging with the caregiver and providers to develop an integrated and holistic plan of care. The clinical case managers support the family by assessing, coordinating, and educating, while also considering the family’s unique physical, social, and cultural needs. A key element addressed by the case manager is solving for social determinants of health issues specific to each family’s situation. Our CM team helps NICU families prepare for their transition to home -- typically connecting with the family within 48 hours of admission into the NICU. We conduct a needs assessment before the infant’s discharge and continue to assess the ongoing clinical needs of the infant throughout the first year of life, including the identification of SDoH issues facing the family. The assessment serves to inform the member-centric plan of care which supports the interventions used by our case managers to solve for any clinical and SDoH issues present throughout the first year.
-
Throughout the entire maternity journey, we support members via voice calls, emails, and text to help ensure a safe, nurturing environment. Our CM team serves as a 24/7 lifeline for support, facilitating access to primary care, answering questions, providing education and appointment reminders, and making connections to community resources to solve SDoH issues.
Our Platform:
We manage the entire continuum of care through Baby Trax®, our purpose-built platform for medically complex infant care that integrates UM, CM, SDoH, and clinical best practices. Using proprietary protocols developed over 16 years and 71,000+ cases, Baby Trax provides a single source of truth for ProgenyHealth’s NICU Care Management program. Baby Trax supports clinical workflows by integrating EHR case data with evidence-based guidelines, prescriptive analytics, and flagging inconsistencies through real-time predictive analytics.
Geo-Mapping for Accessing Community Services to Address SDoH
We use a geo-mapping application to support solving SDoH issues that were identified with the Baby Trax needs assessment. We find validated local resources in real-time and connect families to solutions.
![]() Shelter
Shelter
Solve housing challenges, help apply for housing assistance and for infant Social Security Disability Income
![]() Health Literacy
Health Literacy
Obtain vital resources like breast pump, car seat, and crib; lactation support, behavioral health resources, wellness rewards
![]() Food Insecurity
Food Insecurity
WIC benefits and food stamps, local food banks and faith-based programs
![]()
Transportation
Schedule transportation for initial and ongoing doctor’s visits
![]()
Emotional & Mental Health
Ongoing postpartum care visits, continued screening for signs of depression, connect to social workers
![]() Safety
Safety
Obtain authorization from state custody offices, monitor prescribed Medication-Assisted Treatment (MAT)
![]() Community
Community
Integrated medical and social services are more effective than waiting for families to visit health services
Our People:
ProgenyHealth is a national company dedicated to Maternity and NICU Care Management. We serve women, infants and families along the maternity care continuum, from pregnancy and postpartum to parenting and return to work. We also have a specialized expertise in managing preterm and medically complex births that result in NICU admissions.
With more than 18 years of care management experience, managing nearly 100,000 cases, ProgenyHealth has a distinct vantage point on maternal and infant health. We know that early-stage maternal health plays a significant role in outcomes and alters the long-term health and quality of life for mothers, infants and families.
 Progeny Health’s data-driven Baby Trax platform, coupled with intensive case management and social worker interventions, enables at-risk infants and their caregivers to overcome the most complex SDoH issues. Here’s an example:
Progeny Health’s data-driven Baby Trax platform, coupled with intensive case management and social worker interventions, enables at-risk infants and their caregivers to overcome the most complex SDoH issues. Here’s an example:
Stella and Beatrice – Born at a fragile 26 weeks, premature twins, Stella and Beatrice, needed significant time in the NICU to grow, sleep, and become medically stable. The twins were born during the COVID-19 pandemic to Patricia, a certified nurse’s aide with two toddlers at home. Adding to Patricia’s challenges, the dad was unable to return to the U.S. from overseas due to travel restrictions. Needing to care for her toddlers and avoid her job-related risks from COVID-19, Patricia had no income to create a stable home for her newborns.
Case Management – Our CM team secured rent assistance which freed up rent money for the purchase of food and supplies. Our team also engaged community resources for infant care items, cribs, car seats, and more.
Results – With these pressures lessened, the family was able to better care for their toddlers and devote necessary attention to the care of the preemie twins. This family's story is unique, but they are certainly not alone.
